By Sohail Djariri
Creating an empathetic, holistic health plan member experience can drive improved engagement and help resolve the challenges often associated with healthcare. While resolving healthcare issues is critical to a long-term health plan/member relationship, simplifying the entire healthcare system experience, especially for those taking prescription medications should be at the top of the list.
Timely education and intervention can help health plan members understand prescription benefits, medication costs, and the importance of adhering to a medication regimen. This is especially true for older adults and those with chronic conditions.
A tech-enabled, omnichannel approach ensures that members receive information using the real-time method they prefer: chatbot, self-directed website experience, or a phone call with a live agent. These personalized interactions and real-time solutions cater to every member’s unique needs on their schedule.
Adherence challenges and SDOH
While many reasons exist for medication nonadherence—cost, side effects, communication barriers, complex regimens—many adults 65 years and older cite price as a factor. A nationwide survey of more than 2,000 adults 65 years and older found that slightly more than 20% said high cost often prevented them from taking prescribed medications, according to the JAMA Network Open article. (Cost is among the top reasons that people don’t take medicines, according to the American Medical Association.)
Timely education and intervention can help health plan members understand prescription benefits, medication costs, and the importance of adhering to a medication regimen.
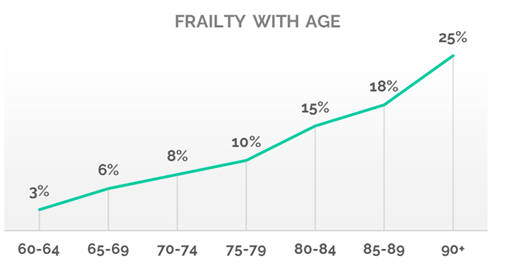
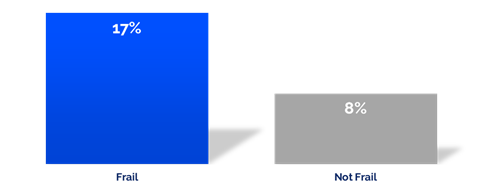
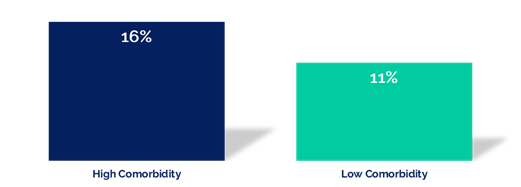
Medication nonadherence in older adults is an important challenge that must be addressed by the healthcare industry. Approximately 89% of those 65 years and older take some type of prescription medicine, according to the Kaiser Family Foundation. Depending on age, explains the Foundation, older adults utilize prescription medication at more than ten times the rate of their younger counterparts.
“Notably, among those who report not taking their medicines as prescribed, slightly more than half (53%) say they didn’t tell their doctor or health care provider (11% of the total) and one-fifth (22%) of this group say their condition got worse as a result of not taking their prescription as recommended (5% of total),” according to the Kaiser Family Foundation.
The responsibility to tackle health equity lies with all of us who work in the healthcare industry, as well as local, state, and federal agencies.
Healthcare access and economics can both impact medication adherence and fall under the domain of the social determinants of health (SDOH). Improving access to healthcare and prescription medication should be a high priority for health plans. Doing so can have positive impacts on health plans, including the ability to:
- Improve member health
- Increase member loyalty
- Drive down costs for chronic conditions
- Make fewer inpatient or emergency department visits
By addressing elements of SDOH, the healthcare industry can get closer to improving health equity for all who participate in the system. A majority of those working in the healthcare industry today say that addressing health equity is critical. “(M)ore than 82 percent of respondents—all of whom work in the health care industry—said that health equity is very or somewhat significant in our health care system today,” according to a Rise to Health Coalition study. “At the same time, less than half of respondents (43.08 percent) said they were either very or somewhat confident the current health care system can effectively address health equity.”
The responsibility to tackle health equity lies with all of us who work in the healthcare industry, as well as local, state, and federal agencies.
Improving member engagement
Older adults appear particularly susceptible to skipping important prescribed medications. Whether it’s cost or a poor understanding of the necessity of the prescription, the healthcare industry must implement programs to address these issues by:
- Building a holistic, team-driven approach to help remedy the cost issue by guiding members toward pharmaceutical company discounts, offering less expensive options, or providing generic medications to reduce costs.
- Utilizing omnichannel communications methods to inform members with easy-to-understand information about the importance of medication adherence.
Member experience programs such as these, as well as others designed to improve communication and understanding between the health plan and its customers, should be explored, and implemented. Much of the infrastructure and technology exists and continues to be improved, allowing health plans to impart knowledge using a variety of accessible and cost-effective tools. With a strategic approach, the healthcare industry can make progress quickly and continue to assist in improving the health of older adults.