Aging in Place Programs Drive Health Plan, Member Benefits
rajath neodesynz
Specialization

By Sohail Djariri
Identifying and mitigating frailty in older adult health plan populations through an aging-in-place-as-a-service solution can help health plans holistically approach this challenging issue in the member population.
A comprehensive solution combines all aspects of the program by creating an end-to-end, long-term view of the participant that relies on health data. The program uses participant information and integrates all operational and technological aspects of the aging-in-place program.
Frailty Definition, Health Plan Impact
Frailty is a condition in older adults characterized by an accumulation of deficits and a loss of physiological reserve which causes increased clinical vulnerability. Frail older adults suffer from multiple deficits across issues like weight loss, fatigue, and slow walking.
The physical and psychological effects on members are considerable; the impact on health plans is also substantial.
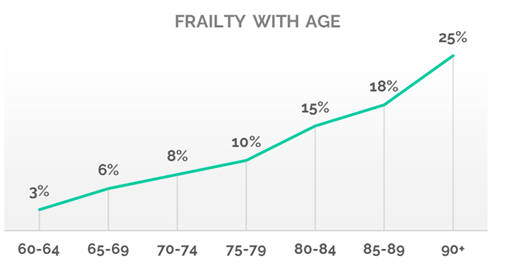
Cutline: Frailty increases with age. Source: Sagility data analysis.
There are several ways that frailty negatively manifests for health plans:
- Frailty is an independent factor contributing to a decline in health and higher utilization of healthcare services.
- The condition is highly prevalent, affecting 17% of those 50 years and older.
- Early frailty identification and intervention are often overlooked in Medicare and special needs plan members.
- Physicians rarely code for weakness, failure to thrive, gait issues, and functional deficits, causing a missed opportunity for health plans.
- Frailty is underreported by 37%, according to Sagility data.
- Electronic medical records don’t prioritize functional status as a priority field, and hierarchical condition category priorities aren’t directly related to frailty.
Frailty Is a Better Predictor of Long-Term Care Needs
Sagility analyzed Centers for Medicare and Medicaid Services data to understand how the use of certain healthcare modalities in older adults can be used to identify frailty. 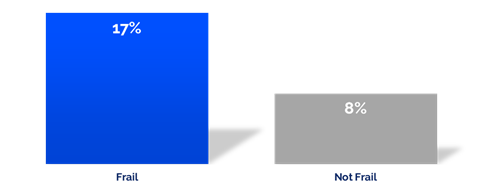
Cutline: Skilled nursing facility and home health cost as a percentage of the total cost of care by frailty indicator. Source: Sagility data analysis.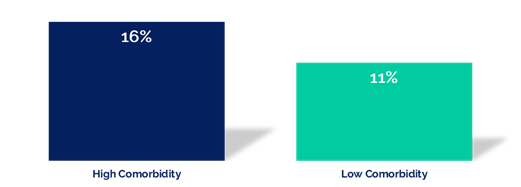
Cutline: Skilled nursing facility and home health cost as a percentage of the total cost of care by clinical indicator. Source: Sagility data analysis.
End-to-End Frailty Program Components
While frailty is a debilitating condition, modification is possible with early identification and targeted interventions. This is achieved through a whole-person program that includes clinical, community, and member communications.
A specialized, end-to-end program enables individuals to age on their own terms in their homes. The program should apply evidence-based assessments with specific clinical interventions designed to identify and address frailty. (Most aging-in-place programs are based on disease state and related comorbidities, rather than interventions that focus on frailty.)
The program elements necessary to launch a holistic approach to aging in place include:
- Frailty predictive analysis: Frailty is the key leading indicator of diminishing health and risk of falls. Using predictive analytics, health plans can identify and enroll members into a frailty program. Modeling also helps identify those members most likely to engage with the program and benefit from long-term participation.
- Evidence-based interventions: Validated screening tools, such as the Tilburg Frailty Indicator assessment, should inform interventions, including care coordination services. These services include physical, behavioral, social, and life factors identification and treatment where appropriate.
- Whole person care approach: This method identifies and addresses the root causes of non-compliance and unhealthy behaviors. It also helps members build resiliency and self-sufficiency.
- Concierge member engagement: This member-focused approach helps build trust and relationships with members through omnichannel engagement. Member-centric clinicians and advocates bring empathy, listening skills, behavior change expertise, and openness to the program. The team also coordinates health plan benefits, including those provided by Medicare.
- Technology platform: While much of an aging-in-place program is provided through a person-to-person approach, just as important is the technology. Health plans should use a highly secure platform with a flexible rules engine to allow seamless program updates and changes, as well as clinical content and workflows. Omnichannel member engagement can include email, a portal, text messages, chatbots, and calls.
Bring It All Together
A holistic approach to an aging-in-place program benefits health plans and members by driving financial, operational, business, and health value.
An aging-in-place program offers many important benefits for older adults, care teams, and health plans:
- Identifies frailty through predictive analytics
- Prevents falls
- Builds resilience in older adults and supports their caregiving team
- Reduces skilled nursing facility admissions and hospital length of stay related to frailty
- Uses community partners to deliver home-based care
- Optimizes coordination of supplementary benefits
- Provides clinically evidenced assessments and interventions using a multi-disciplinary team of clinicians
- Improves Star Ratings
As the number of older adults continues to increase—with nearly 56 million as of the 2020 census—aging-in-place programs with a frailty focus become not only important to this population but mandatory for health plans to remain competitive in the future.
